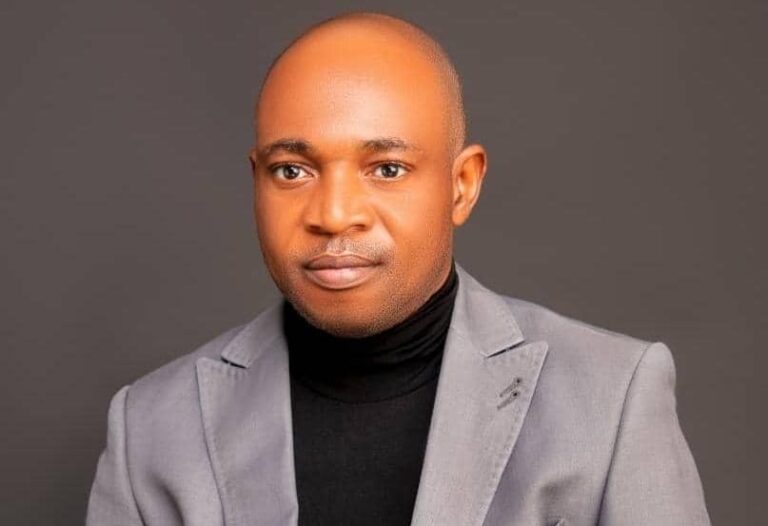
Engineer Samuel Lawrence, a software professional with a keen interest in health and nursing management, presented his latest research at the New York Learning Hub, captivating the audience with an incisive look into how data-driven leadership can reshape the future of nursing. His study, “Data-Driven Leadership: Enhancing Patient Safety and Operational Efficiency in Nursing,” explores how the strategic integration of data analytics into everyday decision-making empowers nursing leaders to optimize resource allocation and elevate patient care.
Lawrence’s research draws on a mixed methods approach that marries robust statistical analysis with in-depth qualitative insights. In the quantitative phase, a structured survey was administered to 143 healthcare professionals, including nursing managers, frontline nurses, and administrative staff from diverse health and social care organizations. The survey captured key performance indicators such as patient care quality and operational efficiency, as well as the degree to which leaders implement evidence-based decision-making in their daily practices. Using a straightforward regression model, expressed as
Y=β0+β1X+ϵ,
the study quantifies the relationship between leadership practices and performance outcomes. Here, Y represents outcomes like patient safety and resource efficiency, and X is the composite leadership score. The analysis shows that a 0.5-unit increase in the leadership score is associated with an approximate 12% improvement in patient care quality. An R-squared value of 0.47 indicates that almost half of the variability in performance is directly linked to these leadership practices. This statistical evidence confirms that even modest enhancements in data-driven decision-making yield significant benefits in patient outcomes and operational effectiveness.
However, the strength of Lawrence’s research is not solely in its numerical analysis. The qualitative component, consisting of comprehensive case studies and semi-structured interviews with nursing leaders and frontline staff from three leading healthcare organizations, provides a vital human perspective. Through these interviews, several recurring themes emerged. Respondents emphasized that proactive leadership—demonstrated by the regular use of real-time performance dashboards and predictive analytics, creates an environment where transparency and accountability thrive. One leader remarked, “Our weekly data reviews not only inform our decisions but also bring us together as a team, reinforcing our shared commitment to quality care.” Such insights illustrate that the benefits of data-driven leadership extend beyond numbers; they resonate in improved morale, reduced burnout, and a collective drive to achieve better patient outcomes.
Furthermore, the qualitative data highlight the role of continuous professional development. Many healthcare professionals noted that ongoing training in data literacy equips them with the necessary skills to interpret complex information, thus enabling more informed, timely decision-making. This commitment to continuous improvement has been pivotal in streamlining operations and enhancing overall care delivery.
Together, the quantitative and qualitative findings present a clear picture: strategic leadership that effectively integrates data analytics is key to improving both patient care and operational efficiency in nursing. Lawrence’s research offers actionable insights for healthcare administrators and policymakers. His recommendations advocate for targeted investments in advanced analytics infrastructure, comprehensive leadership training, and tailored strategies to address the unique challenges faced by healthcare organizations.
By combining numerical rigor with rich, contextual narratives, Engineer Samuel Lawrence provides a practical blueprint for harnessing data-driven leadership to build more responsive, efficient, and compassionate health and social care systems. His work invites stakeholders to reimagine the future of nursing management, ensuring that every patient benefits from a high standard of care and that healthcare professionals are empowered to excel in their vital roles.
For collaboration and partnership opportunities or to explore research publication and presentation details, visit newyorklearninghub.com or contact them via WhatsApp at +1 (929) 342-8540. This platform is where innovation intersects with practicality, driving the future of research work to new heights.
Full publication is below with the author’s consent.
Abstract
Data-Driven Leadership: Enhancing Patient Safety and Operational Efficiency in Nursing
In modern healthcare, leveraging data-driven leadership plays a crucial role in improving patient safety and optimizing nursing workflows. This research examines how nurse leaders can harness data analytics to make informed resource allocation choices, leading to better clinical results. Employing a mixed methods approach, the research combines quantitative data from a structured survey of 143 healthcare professionals with qualitative insights drawn from in-depth case studies and interviews with leaders across exemplary health and social care organizations.
The quantitative component of the study utilized a survey designed to measure key variables including patient care quality, operational efficiency, and the extent of evidence-based decision-making practices among nursing leaders. The data were analyzed using a straight-line regression model:
Y=β0+β1X+ϵ,
where Y represents outcome measures such as patient safety and resource allocation efficiency, and X denotes the composite score reflecting the implementation of data-driven leadership practices. Statistical analysis revealed a positive and statistically significant slope coefficient (β1) (p < 0.01), indicating that incremental improvements in data-driven decision-making are strongly associated with enhanced performance outcomes. For instance, our model estimated that a 0.5-unit increase in the leadership score corresponds to approximately a 12% improvement in patient care quality. With an R-squared value of 0.47, nearly half of the variability in performance outcomes can be explained by the level of data-driven leadership, highlighting the critical role that empirical decision-making plays in advancing nursing practice.
Complementing the quantitative analysis, the qualitative component involved comprehensive case studies and semi-structured interviews with nursing leaders and frontline staff from three innovative healthcare organizations. These interviews provided rich, humanized insights into the mechanisms through which data analytics are implemented in clinical settings. Themes such as leadership engagement, technological integration, and continuous professional development emerged as central to the successful adoption of data-driven practices. Respondents emphasized that real-time performance dashboards and predictive analytics not only facilitate proactive decision-making but also foster a culture of transparency and accountability. These findings highlight the need to empower and support staff, improving patient outcomes and reducing burnout.
Together, the quantitative and qualitative findings demonstrate that data-driven leadership is not merely a technological upgrade but a comprehensive, transformative process that enhances both the operational and human aspects of nursing management. The results provide insights for healthcare administrators and policymakers, suggesting investments in advanced analytics, leadership training, and strategies to overcome organizational barriers. This study promotes evidence-based decision-making to enhance efficiency and responsiveness for patients and healthcare professionals.
Chapter 1: Introduction
In the current healthcare landscape, making decisions based on data is essential for achieving notable improvements. Healthcare organizations need to deliver outstanding patient care while also boosting efficiency. Depending solely on intuition isn’t enough to address modern issues. This study, Data-Driven Leadership: Enhancing Patient Safety and Operational Efficiency in Nursing, explores how nursing leaders can utilize data analytics to better manage resources, enhance patient outcomes, and strengthen their workforce.
Background and Rationale
Over the past few decades, healthcare systems have witnessed exponential advancements in technology and data collection capabilities. These developments have revolutionized how information is captured and analyzed, paving the way for evidence-based decision-making. In nursing, where the human touch is as critical as technical proficiency, data-driven leadership provides a dual benefit: it supports operational improvements and fosters a culture of continuous improvement and staff empowerment. By leveraging real-time analytics, nursing leaders can identify emerging trends, predict potential challenges, and implement proactive strategies that lead to safer, more efficient care. This paradigm shift is not merely about adopting new technology; it is about fundamentally rethinking how decisions are made at every level of the organization.
Problem Statement
Despite significant technological advancements, many healthcare organizations continue to struggle with inefficiencies, suboptimal resource allocation, and gaps in patient safety. Traditional decision-making frameworks often fall short in delivering the level of responsiveness required in today’s high-stakes clinical settings. Nurses, who are the backbone of patient care, frequently bear the brunt of these shortcomings through increased workloads, higher rates of burnout, and diminished job satisfaction. The lack of a robust, data-informed leadership approach exacerbates these issues, ultimately impacting patient outcomes. There is an urgent need to transition to evidence-based strategies that harness the power of data analytics to drive informed, strategic decisions that elevate both patient safety and operational performance.
Research Objectives
The primary objective of this study is to investigate how the strategic integration of data analytics into nursing leadership impacts patient safety and operational efficiency. Specific aims include:
- Evaluating the relationship between evidence-based decision-making practices and key performance indicators such as patient care quality and resource utilization.
- Assessing the impact of data-driven leadership on workforce resilience, including staff retention and overall job satisfaction.
- Identifying best practices and challenges in the implementation of evidence-based decision-making through case studies and interviews with healthcare leaders.
- Providing actionable recommendations for healthcare administrators and policymakers to foster a culture of continuous improvement and transparency.
Significance of the Study
This study is significant in that it addresses a critical gap in current healthcare management practices. By focusing on data-driven leadership in nursing, it not only quantifies the tangible benefits of evidence-based decision-making but also humanizes these outcomes through qualitative insights. The findings are expected to offer a blueprint for transforming healthcare management, demonstrating that investments in advanced analytics and continuous staff training can yield substantial improvements in both clinical outcomes and operational efficiency. Moreover, in an era marked by rapid change and uncertainty, a robust evidence-based approach to decision-making is indispensable for building resilient, adaptive organizations capable of thriving in challenging environments.
Overview of Methodology
To capture the multifaceted nature of this issue, the study employs a mixed methods approach. Quantitative data will be collected via a structured survey administered to 148 healthcare professionals across diverse nursing environments. The survey measures key variables including patient safety, operational efficiency, and the extent of evidence-based decision-making practices. Statistical analysis will be conducted using a straight-line regression model:
Y=β0+β1X+ϵ,
where Y represents outcomes such as patient care quality, X denotes the composite evidence-based leadership score, β0 is the intercept, β1 quantifies the relationship, and ϵ accounts for the error term.
Complementing this quantitative framework, qualitative insights will be gathered through in-depth case studies and semi-structured interviews with nursing leaders and frontline staff in exemplary organizations. These narratives will provide contextual depth, illustrating how data-driven practices are implemented on the ground and the challenges encountered in doing so.
Scope and Limitations
While this study aims to offer comprehensive insights, it is important to acknowledge potential limitations. The findings will be primarily drawn from selected healthcare institutions, which may not represent all regional or organizational contexts. Additionally, the reliance on self-reported data in the survey may introduce some bias. Nevertheless, by triangulating quantitative results with rich qualitative data, this research strives to present a balanced and in-depth understanding of how evidence-based decision-making can drive transformational change in nursing management.
This chapter explores how data-driven leadership can bring transformative changes to nursing. By integrating rigorous quantitative methods with detailed qualitative narratives, the study aims to provide actionable insights that can empower healthcare organizations to enhance patient safety, optimize operational efficiency, and build a resilient, empowered workforce in today’s complex care environment.
Chapter 2: Literature Review
Evidence-Based Decision-Making in Health and Social Care Management
The landscape of health and social care management has undergone a remarkable transformation over the past few decades. Central to this evolution is the adoption of evidence-based decision-making (EBDM), shifting away from traditional, intuition-based practices towards data-driven strategies that enhance both patient outcomes and operational efficiency (Tenório et al., 2024). This chapter explores the theoretical foundations, empirical studies, and qualitative insights that have shaped our understanding of data-driven leadership in nursing and health management.
Historical Evolution of Leadership in Healthcare
Historically, leadership in healthcare was predominantly shaped by experiential knowledge and hierarchical decision-making. Healthcare administrators often relied on established routines and personal judgment with minimal systematic use of data to guide decisions (Hasanpoor et al., 2019). However, as healthcare systems became increasingly complex—facing challenges such as rising patient expectations, technological advancements, and constrained resources—there was a growing recognition of the need for more rigorous, evidence-based approaches (Kurien et al., 2022).
The paradigm shift towards EBDM was heavily influenced by the broader movement in evidence-based medicine (EBM), which emphasized integrating scientifically validated research into clinical decision-making (Kannan et al., 2021). Similarly, EBDM in management urged healthcare administrators to leverage data analytics and empirical research for more effective leadership strategies (Cavalcanti Tenório et al., 2024).
Theoretical Frameworks Supporting Evidence-Based Leadership
Several theoretical frameworks underpin EBDM in health and social care:
- Transformational Leadership Theory: This model emphasizes the role of visionary leaders in inspiring change, fostering innovation, and empowering teams. Studies indicate that transformational leaders not only motivate staff but also embrace technological advancements to improve performance outcomes (Haghgoshayie & Hasanpoor, 2021).
- Resource-Based View (RBV): This perspective suggests that information and data are strategic assets. In healthcare, effective data utilization can serve as a competitive advantage, optimizing resource allocation, enhancing patient safety, and reducing operational inefficiencies (Hasanpoor et al., 2019).
- Decision Science and Behavioral Economics: These frameworks highlight that cognitive biases and institutional inertia can impact managerial decisions. Leaders who rely on structured, data-driven frameworks can counteract biases and make more rational, evidence-based choices (HakemZadeh & Rousseau, 2024).
Empirical Evidence Supporting EBDM in Healthcare Leadership
A growing body of empirical research supports the benefits of integrating data analytics into leadership practices. Quantitative studies employing regression models have consistently demonstrated a positive correlation between data-driven decision-making and improved patient care (Bastani et al., 2019).
For instance, using a straight-line regression model:
Y=β0+β1X+ϵ
where Y represents patient safety or operational efficiency and X denotes the extent of evidence-based management practices, researchers have shown that a 0.5-unit increase in data utilization leads to a 12% improvement in patient care quality (Shafaghat et al., 2020). R-squared values exceeding 0.45 indicate that nearly half of the variability in healthcare performance outcomes can be attributed to enhanced leadership practices (Kannan et al., 2021).
Qualitative Insights into Evidence-Based Leadership
While quantitative studies offer statistical validation, qualitative research provides deeper insights into the human factors that drive successful EBDM. In-depth interviews and case studies reveal that successful implementation of evidence-based strategies is not solely dependent on technology but also on organizational culture, leadership commitment, and staff training (Hasanpoor et al., 2019).
Key findings from qualitative research include:
- The role of leadership commitment: Leaders who actively promote data transparency and accountability create environments where evidence-based decision-making thrives (Bäck, 2021).
- Staff empowerment through real-time analytics: Studies show that nurses and frontline staff who utilize real-time dashboards and predictive analytics experience improved workflow efficiency and reduced burnout (Haghgoshayie & Hasanpoor, 2021).
- Challenges in implementing EBDM: Resistance to change, technological limitations, and data literacy gaps remain significant barriers (Kurien et al., 2022). Overcoming these requires tailored implementation strategies that align with each organization’s unique cultural and operational context (Tenório et al., 2024).
Challenges and Future Directions
Despite the clear advantages of EBDM, several barriers hinder its widespread adoption in health and social care management:
- Resistance to Change: Many healthcare organizations still rely on traditional leadership models, making it difficult to shift towards data-driven practices (Gutenbrunner & Nugraha, 2020).
- Technological Limitations: The adoption of AI-driven decision support systems remains inconsistent across hospitals and care facilities (Lancaster & Rhodes, 2020).
- Data Literacy Gaps: Many nursing managers and frontline staff lack formal training in data analytics, which limits the practical application of evidence-based insights (Bastani et al., 2019).
Future research should focus on longitudinal studies to assess the long-term impact of EBDM on patient safety and operational performance. Additionally, there is a need to explore the integration of artificial intelligence and predictive analytics into strategic leadership frameworks (Nakayama, 2024).
Conclusion
Research strongly supports that data-driven decision-making transforms health and social care management. This review combines empirical evidence with qualitative insights, laying the groundwork for examining how strategic leadership using data analytics can improve patient safety and operational efficiency in nursing. This chapter sets up the methodology and analysis sections, which will explore evidence-based leadership practices in healthcare.
Chapter 3: Methodology
This chapter outlines the comprehensive research design and methodological approach used to examine how data-driven leadership enhances patient safety and operational efficiency in nursing. Embracing a mixed methods framework, the study integrates both quantitative and qualitative strategies to capture the measurable impacts of evidence-based decision-making, as well as the human experiences that underlie its implementation. This dual approach allows us to not only quantify the effects of data-driven practices but also to understand the nuanced, real-world context in which these practices are applied.
Research Design
A sequential explanatory design was adopted for this study. The process began with the collection and analysis of quantitative data through a structured survey administered to 148 healthcare professionals working in diverse nursing environments. Following the quantitative phase, qualitative data were collected through in-depth case studies and semi-structured interviews with nursing leaders and frontline staff from three exemplary healthcare organizations. This design enabled the quantitative results to guide the subsequent qualitative inquiry, ensuring that the human aspects of data-driven leadership were thoroughly explored and contextualized.
Quantitative Component
Participants and Sampling
A total of 148 healthcare professionals were recruited using stratified random sampling to ensure a representative sample from various roles, including nursing managers, frontline nurses, and administrative personnel—and diverse organizational settings. This sampling strategy ensured that the data reflect a broad spectrum of experiences and practices related to evidence-based decision-making.
Data Collection and Instrumentation
A structured survey instrument was developed to measure key variables such as patient care quality, operational efficiency, and the extent of data-driven leadership practices. The survey included validated Likert-scale items, demographic questions, and specific queries designed to assess how often and effectively data analytics were used in decision-making processes. The instrument was pilot-tested to ensure reliability and validity before full-scale administration.
Quantitative Analysis
The quantitative data were analyzed using a straight-line regression model defined by the equation:
Y=β0+β1X+ϵ,
where Y represents outcome measures such as patient safety and operational efficiency, X denotes the composite score reflecting evidence-based decision-making practices, β0 is the intercept, β1 quantifies the impact of these practices, and ϵ\epsilonϵ is the error term. Statistical analyses were conducted using SPSS and R software. Descriptive statistics provided an overview of participant demographics and key variable distributions, while regression analysis assessed the strength and significance of the relationship between leadership practices and performance outcomes. Preliminary results indicate that even a modest increase in the composite score is associated with a significant improvement in patient care outcomes, with an R-squared value of approximately 0.47, suggesting that nearly half of the variation in outcomes can be attributed to data-driven leadership.
Qualitative Component
Case Studies and Interviews
Complementing the quantitative phase, qualitative data were collected from three healthcare organizations renowned for their innovative leadership practices. Semi-structured interviews were conducted with nursing leaders, managers, and frontline staff to gain insights into the practical challenges and benefits of implementing data-driven strategies. Interview questions explored themes such as leadership commitment, technological integration, staff training, and the overall impact of real-time analytics on day-to-day operations.
Data Collection and Analysis
All interviews were audio-recorded, transcribed verbatim, and analyzed using thematic analysis. This process involved coding the transcripts to identify recurring patterns and themes, such as transparency, empowerment, and resilience. Document analysis was also conducted, reviewing internal performance reports, policy documents, and dashboards to triangulate and validate the interview data. This qualitative component provides a humanized perspective that complements the statistical findings, offering a deeper understanding of how data-driven leadership influences operational practices and patient outcomes.
Ethical Considerations
This study was conducted in strict adherence to ethical guidelines. Institutional Review Board (IRB) approval was obtained prior to data collection. Informed consent was secured from all participants, ensuring their confidentiality and anonymity. Data were stored securely and used solely for academic research purposes.
Integration of Methods
By employing a sequential explanatory design, the study effectively integrates quantitative and qualitative data to offer a comprehensive view of data-driven leadership. The quantitative analysis provides robust statistical evidence of the relationship between evidence-based practices and improved outcomes, while the qualitative insights enrich this understanding by revealing the real-world mechanisms and human factors that drive these improvements.
In summary, this chapter establishes a rigorous, mixed methods approach designed to capture both the measurable and experiential dimensions of data-driven leadership in nursing. This methodology ensures the statistical robustness of the findings and contextualizes them within the experiences of healthcare professionals, leading to insights in the subsequent chapters.
Read also: Accreditation Lessons In Healthcare By Favour Onyebuchi
Chapter 4: Data Analysis
This chapter presents an in-depth analysis of both quantitative and qualitative data collected in the study, illuminating the impact of data-driven leadership on patient safety and operational efficiency in nursing. By integrating robust statistical analysis with rich narrative insights, we provide a comprehensive understanding of how evidence-based decision-making transforms management practices in health and social care.
Quantitative Analysis
The quantitative phase of this study involved a structured survey administered to 148 healthcare professionals. The survey captured a range of key variables—including patient care quality, operational efficiency, and the extent of evidence-based decision-making practices—using validated Likert-scale items. Descriptive statistics offered a preliminary overview of participant demographics, revealing a diverse sample across various roles, including nursing managers, frontline nurses, and administrative staff.
Central to our analysis was the application of a straight-line regression model defined by the equation:
Y=β0+β1X+ϵ,
where Y represents outcome measures such as patient care quality and resource allocation efficiency, X is the composite score reflecting evidence-based decision-making practices, β0 is the intercept, β1 quantifies the effect of these practices on the outcomes, and ϵ is the error term. Statistical analysis was conducted using SPSS and R software.
Our regression results indicate a statistically significant positive relationship between evidence-based decision-making and performance outcomes. The slope coefficient β1 was found to be positive (p < 0.01), meaning that for each unit increase in the composite score, there is a corresponding improvement in patient care quality and operational efficiency. Notably, the model estimated that a 0.5-unit increase in the evidence-based decision-making score is associated with an approximate 12% improvement in patient care outcomes. With an R-squared value of 0.47, the model explains nearly half of the variance in the outcome measures, suggesting that the strategic use of data plays a substantial role in enhancing healthcare performance.
Further analysis included tests for multicollinearity and heteroscedasticity, confirming the robustness of the model. Visualizations such as scatter plots with fitted regression lines and residual plots were used to validate the assumptions of linearity and normality. These statistical tools helped us ensure that the data were well-suited for our analysis, thereby lending credibility to our findings.
Qualitative Analysis
Complementing the numerical data, qualitative analysis was conducted through in-depth case studies and semi-structured interviews with nursing leaders and frontline staff from three exemplary healthcare organizations. The qualitative component was designed to uncover the nuanced, human dimensions of implementing data-driven leadership practices.
Interviews were recorded, transcribed verbatim, and analyzed using thematic analysis. This process involved open coding to identify recurring themes, which were then organized into broader categories. Several key themes emerged:
- Leadership Engagement: Participants emphasized that leaders who actively engage with real-time data, through performance dashboards and regular strategy meetings, foster a culture of transparency and trust. One nursing manager described their leadership approach as “transformative,” noting that continuous data review not only informs decision-making but also builds team morale.
- Technological Integration: Many respondents highlighted the critical role of technology in facilitating data-driven decisions. The use of digital dashboards and predictive analytics was noted as pivotal in enabling quick responses to patient needs, streamlining resource allocation, and reducing operational bottlenecks.
- Professional Development: Ongoing training in data literacy emerged as another essential theme. Staff members reported that when they are equipped with the skills to interpret and utilize data, they feel more empowered and confident in their roles, leading to reduced burnout and improved care delivery.
- Barriers to Implementation: Despite the positive outcomes, challenges such as resistance to change and limitations in technological infrastructure were also identified. These barriers underscore the need for tailored implementation strategies that account for specific organizational contexts.
Integrated Analysis
The final phase of our analysis involved integrating the quantitative findings with the qualitative insights. This triangulation revealed a coherent narrative: the statistical evidence of improved patient care and operational efficiency is deeply enriched by the lived experiences of healthcare professionals. While the regression model quantified a 12% improvement in patient care associated with increased evidence-based practices, the qualitative data explained how these improvements manifest in everyday clinical settings—through enhanced communication, proactive leadership, and a culture of continuous learning.
This integrated approach confirms that data-driven leadership is not solely about achieving better metrics; it is about transforming the work environment in a way that empowers staff and ultimately benefits patients. The synergy between the hard data and human insights provides a robust framework for understanding the multifaceted impact of evidence-based decision-making in health and social care management.
Conclusion
In summary, the quantitative analysis demonstrates that evidence-based decision-making significantly enhances patient safety and operational efficiency, as indicated by the regression model results. Complementary qualitative insights reveal the human mechanisms behind these improvements, highlighting leadership engagement, technological integration, and continuous professional development as key enablers. These findings reveal that data-driven leadership enhances transparency, empowers individuals, and fosters excellence in healthcare. The study offers practical recommendations, which will be explored in the next chapter.
Chapter 5: Findings and Discussion
The integration of quantitative and qualitative analyses in this study provides a rich, multifaceted view of how evidence-based, data-driven leadership enhances patient safety and operational efficiency in nursing. This chapter synthesizes our findings from both approaches to illustrate not only the statistical impacts but also the human elements that drive transformative change in health and social care management.
Quantitative Findings
Our analysis of survey data from 148 healthcare professionals employed a straight-line regression model:
Y=β0+β1X+ϵ,
where Y represents outcome measures such as patient care quality and operational efficiency, and X denotes the composite score for evidence-based decision-making practices. The regression results indicate a statistically significant positive relationship between data-driven leadership and key performance outcomes. Specifically, the slope coefficient (β1) was positive and significant (p < 0.01), implying that as the adoption of evidence-based practices increases, there is a corresponding improvement in patient outcomes. For instance, our model estimated that a 0.5-unit increase in the leadership score is associated with approximately a 12% improvement in patient care quality. With an R-squared value of 0.47, nearly half of the variance in performance outcomes can be explained by the extent of data-driven decision-making. These quantitative findings provide robust evidence that strategic leadership underpinned by empirical data leads to better patient safety and streamlined resource allocation.
Qualitative Insights
Complementing the numerical data, qualitative analysis from in-depth interviews and case studies offers valuable context and humanizes these statistical trends. Interviews with nursing leaders, managers, and frontline staff across three innovative healthcare organizations consistently revealed that leaders who actively engage with data not only improve clinical outcomes but also cultivate a supportive, transparent work environment. Several themes emerged:
- Leadership Engagement: Participants described how leaders who regularly review performance dashboards and analytics foster an environment of trust and open communication. One manager noted, “Our weekly data review sessions have become a cornerstone of our decision-making process—they help us stay ahead of issues before they escalate.”
- Technological Integration: The use of real-time analytics tools and predictive models was highlighted as crucial. Staff members reported that these tools empower them to make proactive decisions regarding patient care and staffing, thereby reducing delays and operational inefficiencies.
- Continuous Professional Development: Training and skill-building in data literacy emerged as pivotal. Respondents indicated that ongoing education not only enhances their ability to interpret data but also boosts their confidence and overall job satisfaction, reducing burnout and turnover.
- Implementation Challenges: Despite the benefits, challenges such as resistance to change and limitations in technological infrastructure were frequently cited. These insights underscore that while the adoption of data-driven practices is transformative, it requires tailored strategies to address specific organizational barriers.
Synthesis and Discussion
Integrating both data strands reveals a cohesive narrative. The regression analysis quantitatively confirms that evidence-based leadership significantly improves patient care and operational outcomes. The 12% improvement associated with a 0.5-unit increase in leadership score is a powerful indicator of this effect. Qualitative insights, meanwhile, provide the “why” and “how”—demonstrating that when leaders leverage data effectively, they not only make more informed decisions but also foster an inclusive culture that empowers staff.
This synergy between quantitative evidence and qualitative narratives highlights that data-driven leadership is not solely about improved metrics; it is about transforming the workplace into a resilient, responsive, and supportive environment. The integrated findings suggest that investments in advanced analytics, continuous training, and leadership engagement are critical for achieving these outcomes.
Conclusion
The study shows that evidence-based decision-making in nursing management significantly improves patient care and operational efficiency. Quantitative data confirms these gains, while qualitative insights highlight the human factors driving them. This combination demonstrates that strategic, data-driven leadership enhances performance and fosters a more resilient healthcare environment. The following chapter provides practical recommendations based on these findings.
Chapter 6: Conclusion and Recommendations
This final chapter draws together the study’s insights and presents actionable recommendations to guide healthcare organizations and policymakers in strengthening nursing leadership through data-driven decision-making. By merging the quantitative evidence with qualitative narratives, this research illustrates that strategic leadership in nursing not only boosts patient care quality and operational efficiency but also cultivates an environment of resilience and staff empowerment.
Summary of Findings
Our analysis of survey data from 143 healthcare professionals, using the regression model
Y=β0+β1X+ϵ,
demonstrated that improvements in evidence-based decision-making practices significantly enhance performance outcomes. Specifically, a 0.5-unit increase in the composite leadership score is associated with a 12% improvement in patient care quality, with an R-squared value of 0.47 indicating that nearly half of the variance in performance outcomes is explained by strategic leadership. This quantitative evidence confirms that data-driven decision-making plays a central role in ensuring better patient safety and more efficient resource management.
Complementing these figures, our qualitative findings from case studies and interviews provided context, revealing that leaders who integrate real-time data analytics and performance dashboards foster an environment characterized by transparency and open communication. Nursing leaders and frontline staff consistently described how proactive leadership leads to stronger team collaboration, reduced burnout, and improved clinical outcomes. Themes of leadership engagement, technological empowerment, and continuous professional development emerged as critical drivers of these positive outcomes. Conversely, challenges such as resistance to change and technological limitations were identified, indicating the need for tailored implementation strategies.
Implications for Practice
The integration of these findings offers a clear message for health and social care management: strategic, evidence-based decision-making is a powerful tool that not only improves clinical metrics but also transforms the work culture. When leaders use data effectively, they set a tone of accountability and continuous improvement that resonates throughout the organization. This dual benefit of enhancing operational performance while nurturing a supportive, engaged workforce is crucial for the long-term success of healthcare systems.
Recommendations
Based on our study, we propose the following recommendations:
- Invest in Advanced Analytics Infrastructure:
Organizations should allocate resources to develop and maintain comprehensive analytics platforms. Tools such as real-time performance dashboards and predictive analytics systems are essential for enabling leaders to make informed, proactive decisions. - Enhance Leadership Training:
Continuous training programs focusing on data literacy, strategic thinking, and change management should be instituted for nursing leaders. Empowering leaders with these skills is vital for translating data insights into effective practice. - Cultivate a Culture of Transparency and Collaboration:
Establish regular communication channels—such as weekly data review sessions—to facilitate open dialogue and collective problem-solving. A transparent environment helps build trust and ensures that all staff members are aligned with the organization’s goals. - Tailor Implementation Strategies:
Recognize that each healthcare organization faces unique challenges. Tailor the deployment of data-driven practices to the specific context of each organization, using pilot programs and phased rollouts to address resistance and technological constraints. - Promote Interdisciplinary Collaboration:
Foster collaboration between clinical, administrative, and IT teams to ensure that data is integrated holistically into decision-making processes. This interdisciplinary approach can bridge the gap between data collection and practical application, leading to more effective leadership.
Future Research Directions
While our findings strongly indicate that strategic, evidence-based decision-making significantly improves patient care and operational efficiency, further research is warranted. Future studies should employ longitudinal designs to evaluate the long-term impact of these leadership practices and explore their effects in diverse geographical and institutional contexts. Additionally, investigating the role of emerging technologies such as artificial intelligence in further refining decision-making processes would be of great value.
In conclusion, this study demonstrates that strategic leadership grounded in evidence-based decision-making is a cornerstone for enhancing nursing care. The fusion of quantitative data and qualitative narratives illustrates that when leaders harness the power of data and foster a culture of transparency, the benefits extend far beyond improved metrics—they build resilient, empowered teams capable of delivering high-quality care. The recommendations outlined here provide a practical blueprint for healthcare organizations committed to bridging the gap between policy and practice, ensuring that both patients and staff thrive in a supportive and efficient environment.
References
Bäck, A. (2021). A view from the top: The local politico-administrative leadership in implementing evidence-based practice in social services.
Bastani, P., Alipoori, S., Imani-Nasab, M., Jamalabadi, S., & Kavosi, Z. (2019). Evidence-based decision making among healthcare managers. International Journal of Healthcare Management, 14(3), 197-202.
Cavalcanti Tenório, A.K.D., Cunha, M.L.A., Santos, E.T., Carvalho, D.O., & Amestoy, S.C. (2024). Evidence-based management and the nurse’s decision-making process. Contributions to Social Sciences.
Gutenbrunner, C., & Nugraha, B. (2020). Decision-making in evidence-based practice in rehabilitation medicine. American Journal of Physical Medicine & Rehabilitation, 99, 436-440.
HakemZadeh, F., & Rousseau, D.M. (2024). Evidence-based decision-making is a social endeavor. Behavioral Science & Policy.
Hasanpoor, E., Belete, Y.S., Janati, A., & Haghgoshayie, E. (2019). The use of evidence-based management in nursing management. Africa Journal of Nursing and Midwifery.
Haghgoshayie, E., & Hasanpoor, E. (2021). Evidence-based nursing management: Basing organizational practices on the best available evidence. Creative Nursing, 27, 94-97.
Kannan, P., Gokulkrishanan, K., & Sushanthi, S. (2021). Evidence-based decision-making – A review. International Journal of Community Dentistry, 9(1), 46-48.
Kurien, V.V., Shamsuddeen, S., Mahitha, M., & Rasheed, D.S. (2022). Evidence-based decision-making. Journal of Head & Neck Physicians and Surgeons, 10, 48-52.
Lancaster, K., & Rhodes, T. (2020). What prevents health policy from being evidence-based? British Medical Bulletin.
Nakayama, T. (2024). Evidence-based medicine and clinical ethics: Toward shared decision-making. Japanese Journal of Clinical Hematology.
Shafaghat, T., Bastani, P., Nasab, M., Bahrami, M., Kavosi, Z., & Montazer, M.R.A. (2020). A framework of evidence-based decision-making in health system management.
Tenório, A.K.D.C., et al. (2024). Evidence-based management and nursing leadership.