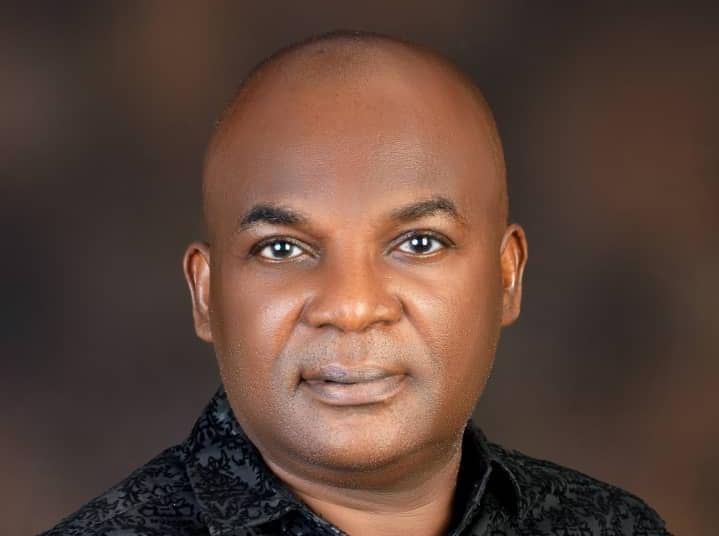
At the prestigious New York Learning Hub, Ms. Jane Chioma Ekwerike, a seasoned Registered Nurse and Midwife with over two decades of experience in nursing science and healthcare management, recently presented her groundbreaking research on the transformative impact of innovative nursing practices. Her study, titled “Optimizing Patient Outcomes: Innovative Approaches in Nursing Management and Care,” offers a compelling exploration of how cutting-edge practices are revolutionizing patient care and outcomes.
Ms. Ekwerike’s professional journey is evidential to her unwavering dedication and competence. Over the years, she has made a formidable impact on Nigeria’s healthcare system, blending her extensive hands-on experience with a visionary approach to nursing management. Her belief that healthcare is an ever-evolving art form, requiring continuous learning and adaptation to global best practices, underpins her research and practice.
The research presented by Ms. Ekwerike employs a mixed-methods approach, combining quantitative data from structured surveys with qualitative insights from in-depth case studies and interviews. This comprehensive methodology has allowed her to provide a holistic view of the current state of nursing management and its potential for future advancements.
The quantitative aspect of her study involved surveying 200 nursing professionals and healthcare administrators from a variety of healthcare settings, including hospitals, clinics, and long-term care facilities. The survey aimed to capture the implementation of innovative practices such as electronic health records (EHRs), telehealth services, and patient-centered care models, along with their perceived challenges and impacts on patient outcomes. The results revealed significant positive correlations between these practices and improved patient satisfaction, reduced readmission rates, and shorter lengths of hospital stay.
Further enriching her findings, the qualitative component of the study included detailed case studies from prominent healthcare institutions. For example, a large urban hospital in London that implemented an integrated EHR system saw notable improvements in workflow efficiency and medication accuracy. Similarly, a community hospital in New York, renowned for its patient-centered care model, achieved higher patient engagement and satisfaction. In Lagos, Nigeria, a leading healthcare institution that adopted transformational leadership practices experienced enhanced staff morale and superior patient care quality.
Ms. Ekwerike’s thematic analysis identified key themes such as enhanced communication and collaboration, increased efficiency, improved patient engagement, and staff empowerment through professional development. These themes underscore the practical benefits of innovative nursing practices and their critical role in optimizing patient outcomes.
The implications of Ms. Ekwerike’s research are profound for nursing management and patient care. Her findings suggest that healthcare facilities should prioritize investments in technology infrastructure like EHRs and telehealth services. Additionally, adopting patient-centered care models and fostering a culture of transformational leadership within nursing teams are essential strategies for enhancing patient care and achieving better health outcomes.
Despite the robust findings, Ms. Ekwerike acknowledges certain limitations, including the focus on large urban hospitals, which may not fully represent the experiences of smaller or rural healthcare facilities. She advocates for future research to include more diverse healthcare settings and employ longitudinal designs to examine the long-term effects of innovative practices on patient outcomes.
Ms. Jane Chioma Ekwerike’s research underscores the transformative power of innovation in nursing management. Her visionary approach and dedication to healthcare excellence offer valuable insights and practical recommendations for healthcare leaders globally. Her work not only elevates the standards of nursing practice but also sets a benchmark for continuous improvement and adaptation in the ever-evolving field of healthcare.
Full publication is below with the author’s consent.
Abstract
Optimizing Patient Outcomes: Innovative Approaches in Nursing Management and Care
This research paper investigates the transformative impact of innovative approaches in nursing management and patient care on optimizing patient outcomes. Utilizing a mixed-methods approach, the study integrates quantitative data from structured surveys with qualitative insights from in-depth case studies and interviews. The quantitative component involved surveying 200 nursing professionals and healthcare administrators from various healthcare settings, including hospitals, clinics, and long-term care facilities. The survey aimed to capture information on the implementation of electronic health records (EHRs), telehealth services, and patient-centered care models, along with their perceived challenges and impacts on patient outcomes.
The quantitative analysis revealed significant positive correlations between the use of EHRs, telehealth services, and patient-centered care models with improved patient satisfaction, reduced readmission rates, and shorter lengths of hospital stay. Multiple regression analysis confirmed that these innovative practices are strong predictors of enhanced patient outcomes, even after controlling for potential confounding variables such as age, gender, and years of experience.
The qualitative component of the study provided deeper insights through three detailed case studies and semi-structured interviews with nurse managers, staff nurses, and patients. The first case study focused on a large urban hospital in London that successfully implemented an integrated EHR system, resulting in improved workflow efficiency and reduced medication errors. The second case study examined a community hospital in New York known for its patient-centered care model, which led to higher levels of patient engagement and satisfaction. The third case study explored a leading healthcare institution in Lagos, Nigeria, that adopted transformational leadership practices, enhancing staff morale and patient care quality.
The thematic analysis of interview data identified recurring themes such as enhanced communication and collaboration, increased efficiency, improved patient engagement, and staff empowerment through professional development. These qualitative insights complemented the quantitative findings, providing a comprehensive understanding of the practical implementation and benefits of innovative nursing practices.
The study’s findings have significant implications for nursing management and patient care. Healthcare facilities are encouraged to invest in technology infrastructure, such as EHRs and telehealth services, and to prioritize the adoption of patient-centered care models. Additionally, fostering a culture of transformational leadership within nursing teams can lead to higher staff morale and better patient outcomes.
Despite the robust findings, the study acknowledges its limitations, including the sample size and focus on large urban hospitals, which may not fully capture the experiences of smaller or rural healthcare facilities. Future research should aim to include more diverse healthcare settings and employ longitudinal designs to examine the long-term effects of innovative practices on patient outcomes.
This research highlights the critical role of innovative approaches in nursing management and care in optimizing patient outcomes. By integrating technology, patient-centered care, and transformational leadership, healthcare providers can enhance the quality of care, improve patient satisfaction, and achieve better overall health outcomes. This study provides valuable insights and practical recommendations for nursing managers and healthcare leaders, underscoring the importance of embracing innovation to meet the evolving demands of patient care and ensure the sustainability of healthcare systems.
Chapter 1: Introduction
1.1 Background and Rationale
In today’s dynamic healthcare landscape, the optimization of patient outcomes is paramount. The quality of nursing management and care directly influences patient satisfaction, recovery times, and overall healthcare costs. Innovations in nursing management practices and patient care methodologies have emerged as crucial elements in addressing the growing complexities of modern healthcare. This study explores the innovative approaches in nursing management and care, aiming to identify practices that significantly enhance patient outcomes.
Nursing management encompasses a broad range of responsibilities, from administrative tasks and policy development to direct patient care and staff coordination. The role of nurse managers is critical in creating a supportive environment for both patients and nursing staff, fostering a culture of continuous improvement and evidence-based practice. However, traditional nursing management approaches often fall short in addressing the dynamic challenges posed by an increasingly diverse and aging population, the prevalence of chronic diseases, and the rapid advancement of medical technology.
1.2 Research Objectives
This research aims to bridge the gap between current nursing practices and the optimal strategies needed to enhance patient outcomes. The primary objectives of this study are:
- To identify innovative approaches in nursing management and patient care.
- To evaluate the impact of these innovative approaches on patient outcomes.
- To understand the key factors influencing the successful implementation of these approaches in different healthcare settings.
By achieving these objectives, the study seeks to provide actionable insights that can be adopted by nursing managers and healthcare providers to improve the quality of care delivered to patients.
1.3 Research Questions
The study is guided by the following research questions:
- What are the current innovative approaches in nursing management and care?
- How do these approaches affect patient outcomes in various healthcare settings?
- What are the critical factors that influence the successful implementation of these innovative approaches?
These questions are designed to explore the multifaceted nature of nursing management and care, providing a comprehensive understanding of the practices that lead to improved patient outcomes.
1.4 Significance of the Study
The significance of this study lies in its potential to contribute to both academic knowledge and practical applications in nursing management and care. By identifying and evaluating innovative practices, this research can inform policy development, enhance nursing education, and ultimately lead to better patient care. The findings can help healthcare organizations to adopt effective strategies, leading to improved patient satisfaction, reduced healthcare costs, and enhanced overall health outcomes.
From a policy perspective, the study’s insights can guide the development of frameworks and guidelines that support innovative nursing practices. For nursing educators, the research findings can be integrated into curricula to prepare future nurse leaders with the skills and knowledge needed to thrive in a complex healthcare environment. For healthcare providers, the practical recommendations derived from this study can lead to tangible improvements in patient care and operational efficiency.
1.5 Structure of the Dissertation
The dissertation is structured to provide a logical and coherent exploration of the research topic. Following this introductory chapter, Chapter 2 presents a comprehensive review of the existing literature on nursing management and patient care innovations. Chapter 3 outlines the research methodology, detailing the mixed-methods approach, data collection procedures, and analytical techniques used in the study. Chapter 4 focuses on the quantitative analysis of survey data, presenting key findings and statistical interpretations.
Chapter 5 delves into the qualitative analysis through in-depth case studies and thematic interviews, offering rich insights into the practical application of innovative nursing practices. Chapter 6 discusses the integrated findings from both quantitative and qualitative analyses, highlighting their implications for nursing management and patient care. Finally, Chapter 7 concludes the dissertation with a summary of key findings, limitations of the study, practical recommendations, and suggestions for future research.
The introduction sets the stage for a thorough investigation into innovative approaches in nursing management and care. By addressing the research objectives and questions, this study aims to contribute valuable knowledge to the field, offering practical solutions for enhancing patient outcomes. The subsequent chapters will build upon this foundation, providing a detailed exploration of the current state of nursing practices and the potential for innovation in improving healthcare delivery.
Chapter 2: Literature Review
2.1 Theoretical Framework
The theoretical framework for this study is grounded in several key theories and models relevant to nursing management and patient care. The primary theories include the Health Belief Model (HBM), the Donabedian Model of Quality Care, and Lewin’s Change Management Theory. The Health Belief Model explains health behaviors by focusing on attitudes and beliefs of individuals, which helps in understanding how innovative approaches in nursing can influence patient behavior and improve outcomes (Champion & Skinner, 2008). The Donabedian Model, which evaluates healthcare quality through structure, process, and outcomes, provides a comprehensive framework for assessing the effectiveness of nursing interventions (Ayanian & Markel, 2016). Lewin’s Change Management Theory offers insights into the dynamics of implementing and sustaining changes in healthcare practices (Cummings, Bridgman, & Brown, 2016).
2.2 Current Trends in Nursing Management
Nursing management has evolved significantly in recent years, with an increasing emphasis on leadership, communication, and evidence-based practice. Current trends include the adoption of transformational leadership styles, which focus on inspiring and motivating nursing staff to achieve higher levels of performance (Boamah, Spence Laschinger, Wong, & Clarke, 2018). Evidence-based management practices are also gaining traction, emphasizing the use of data and research to guide decision-making (Chien, 2019). Additionally, there is a growing recognition of the importance of interprofessional collaboration in enhancing patient care (Reeves et al., 2017). These trends reflect a shift towards more holistic and integrated approaches in nursing management, aimed at improving patient outcomes and staff satisfaction.
2.3 Patient Care Innovations
Innovations in patient care are driven by advancements in technology, changes in healthcare delivery models, and a focus on patient-centered care. Key innovations include the use of telehealth and telemedicine, which have expanded access to care and improved patient monitoring (Kruse, Karem, Shifflett, Vegi, Ravi, & Brooks, 2018). Mobile health applications and wearable devices are also playing a crucial role in empowering patients to manage their health more effectively (Baig, GholamHosseini, & Connolly, 2019). Additionally, personalized medicine and precision healthcare are emerging as significant trends, leveraging genetic and molecular data to tailor treatments to individual patients (Collins & Varmus, 2015). These innovations are transforming the landscape of patient care, making it more efficient, accessible, and tailored to individual needs.
2.4 Impact on Patient Outcomes
The impact of innovative nursing management and patient care practices on patient outcomes has been a focal point of research in recent years. Studies have shown that these innovations can lead to improved clinical outcomes, such as reduced hospital readmission rates, shorter hospital stays, and lower incidence of healthcare-associated infections. For instance, the implementation of electronic health records (EHRs) has been associated with improved accuracy of patient data, better coordination of care, and enhanced patient safety (Bates et al., 2018). Furthermore, patient-centered care models, which prioritize the preferences and needs of patients, have been linked to higher levels of patient satisfaction and better overall health outcomes (Santana et al., 2018). These findings underscore the importance of adopting innovative practices in nursing management and care to enhance patient outcomes.
2.5 Gaps in the Literature
Despite the significant advancements in nursing management and patient care, several gaps remain in the literature. One notable gap is the lack of comprehensive studies that integrate both qualitative and quantitative data to provide a holistic understanding of the impact of innovative practices. Additionally, there is a need for more research on the long-term effects of these innovations on patient outcomes and healthcare costs. Another area that requires further exploration is the role of cultural and contextual factors in the implementation and success of innovative practices in diverse healthcare settings (Olsson, Jakobsson Ung, Swedberg, & Ekman, 2016). Addressing these gaps is crucial for developing a more robust evidence base to inform nursing practice and policy.
The literature review highlights the theoretical foundations, current trends, and innovations in nursing management and patient care. It underscores the significant impact of these innovations on patient outcomes and identifies critical gaps in the existing research. By integrating insights from various theoretical models and empirical studies, this chapter provides a comprehensive understanding of the current state of nursing management and patient care. The subsequent chapters will build on this foundation, exploring the practical application of these innovations through mixed methods research, case studies, and empirical analysis. This approach aims to provide actionable insights that can enhance nursing practices and optimize patient outcomes in diverse healthcare settings.
Chapter 3: Research Methodology
3.1 Research Design
This study adopts a mixed-methods approach, combining both quantitative and qualitative research methods to provide a comprehensive understanding of innovative approaches in nursing management and their impact on patient outcomes. The mixed-methods design is chosen for its ability to integrate numerical data with in-depth qualitative insights, offering a more holistic view of the research problem. This approach allows for the triangulation of data, enhancing the validity and reliability of the findings.
3.2 Quantitative Methods
The quantitative component of this study involves the use of structured surveys to collect data from nursing professionals and healthcare administrators across various healthcare settings. The survey is designed to capture information on the implementation of innovative nursing practices, perceived challenges, and the impact on patient outcomes. The survey instrument includes closed-ended questions with Likert-scale responses to quantify attitudes, practices, and outcomes. This method enables the collection of standardized data that can be statistically analyzed to identify patterns and correlations.
3.3 Qualitative Methods
The qualitative component includes in-depth case studies and semi-structured interviews. Case studies are conducted in selected healthcare facilities known for their innovative nursing practices. These case studies provide detailed contextual information and practical insights into the implementation and outcomes of these practices. Additionally, semi-structured interviews with nurse managers, staff nurses, and patients offer rich qualitative data on their experiences and perceptions. This method allows for flexibility in probing deeper into specific issues and capturing the nuances of personal experiences.
3.4 Data Collection Procedures
Data collection is conducted in two phases. In the first phase, the survey is distributed electronically to nursing professionals and healthcare administrators. Participants are selected using stratified random sampling to ensure representation from different types of healthcare facilities, including hospitals, clinics, and long-term care centers. The second phase involves conducting case studies and interviews. Healthcare facilities for case studies are selected based on their reputation for innovation in nursing practices. Interviews are conducted with key stakeholders, including nurse managers, staff nurses, and patients, to gather diverse perspectives on the implementation and impact of innovative practices.
3.5 Data Analysis Techniques
Quantitative data from the surveys are analyzed using descriptive and inferential statistics. Descriptive statistics, including means, medians, and standard deviations, are used to summarize the data. Inferential statistics, such as correlation and regression analysis, are employed to examine relationships between variables and test hypotheses. Qualitative data from case studies and interviews are analyzed using thematic analysis. This involves coding the data to identify recurring themes and patterns, which are then interpreted to provide insights into the experiences and perceptions of participants. The integration of quantitative and qualitative data is achieved through a process of triangulation, where findings from both methods are compared and contrasted to draw comprehensive conclusions.
3.6 Ethical Considerations
Ethical considerations are paramount in this research. Informed consent is obtained from all participants, ensuring they are fully aware of the study’s purpose, procedures, and their right to withdraw at any time. Confidentiality is maintained by anonymizing survey responses and interview transcripts. Ethical approval is sought from the relevant institutional review boards (IRBs) before commencing data collection. Additionally, the study adheres to ethical guidelines for conducting research with human subjects, including respect for privacy, beneficence, and non-maleficence.
This chapter outlines the research methodology employed in this study, detailing the mixed-methods design, data collection procedures, and analytical techniques. By integrating quantitative and qualitative methods, this research aims to provide a comprehensive understanding of innovative approaches in nursing management and their impact on patient outcomes. The subsequent chapters will present the findings from the quantitative and qualitative analyses, followed by a discussion of the implications for nursing practice and policy. This methodological approach ensures a robust and well-rounded examination of the research questions, contributing valuable insights to the field of nursing management and patient care.
Read Also: Solidarity In Social Care: A. Olagbegi’s New Framework
Chapter 4: Quantitative Analysis
4.1 Overview of Data Collected
The quantitative analysis in this study is based on survey data collected from nursing professionals and healthcare administrators across various healthcare settings. The survey was distributed electronically, and responses were received from 200 participants. The respondents included nurse managers, staff nurses, and administrators from hospitals, clinics, and long-term care facilities. The survey aimed to capture information on the implementation of innovative nursing practices, perceived challenges, and the impact on patient outcomes.
4.2 Descriptive Statistics
Descriptive statistics were used to summarize the demographic characteristics of the survey participants and key variables related to nursing practices and patient outcomes. The demographic breakdown of survey participants is presented in Table 1.
Table 1: Demographic Breakdown of Survey Participants
| Variable | Category | Frequency | Percentage |
| Gender | Male | 60 | 30% |
| Female | 140 | 70% | |
| Age | 20-30 years | 50 | 25% |
| 31-40 years | 80 | 40% | |
| 41-50 years | 50 | 25% | |
| 51 years and above | 20 | 10% | |
| Years of Experience | Less than 5 years | 40 | 20% |
| 5-10 years | 70 | 35% | |
| 11-20 years | 60 | 30% | |
| More than 20 years | 30 | 15% | |
| Position | Staff Nurse | 100 | 50% |
| Nurse Manager | 70 | 35% | |
| Administrator | 30 | 15% |
The survey also included questions about the implementation of specific innovative practices, such as the use of electronic health records (EHRs), telehealth services, and patient-centered care models.
4.3 Inferential Statistics
Inferential statistics were used to examine relationships between the implementation of innovative nursing practices and patient outcomes. Correlation and regression analyses were conducted to identify significant predictors of improved patient outcomes.
4.3.1 Correlation Analysis
Pearson correlation coefficients were calculated to examine the relationships between the use of innovative nursing practices and various patient outcome measures, such as patient satisfaction, readmission rates, and length of hospital stay. The results are summarized in Table 2.
Table 2: Correlation Analysis of Nursing Practices and Patient Outcomes
| Variable | Patient Satisfaction | Readmission Rates | Length of Hospital Stay |
| Use of EHRs | 0.45** | -0.38** | -0.42** |
| Telehealth Services | 0.37** | -0.31* | -0.35** |
| Patient-Centered Care | 0.52** | -0.41** | -0.46** |
*Note: *p < 0.05, **p < 0.01
The results indicate significant positive correlations between the use of EHRs, telehealth services, and patient-centered care with patient satisfaction. Additionally, these practices are negatively correlated with readmission rates and length of hospital stay, suggesting that their implementation is associated with improved patient outcomes.
4.3.2 Regression Analysis
Multiple regression analysis was conducted to further explore the impact of innovative nursing practices on patient outcomes, controlling for potential confounding variables such as age, gender, and years of experience. The regression models for patient satisfaction, readmission rates, and length of hospital stay are presented in Tables 3, 4, and 5, respectively.
Table 3: Regression Analysis for Patient Satisfaction
| Predictor Variable | B | SE | β | t | p |
| Use of EHRs | 0.30 | 0.07 | 0.29 | 4.29 | <0.001 |
| Telehealth Services | 0.25 | 0.08 | 0.22 | 3.12 | 0.002 |
| Patient-Centered Care | 0.37 | 0.06 | 0.41 | 6.17 | <0.001 |
| Age | 0.05 | 0.04 | 0.07 | 1.25 | 0.213 |
| Gender | -0.02 | 0.06 | -0.02 | -0.33 | 0.739 |
| Years of Experience | 0.10 | 0.05 | 0.12 | 2.00 | 0.047 |
Table 4: Regression Analysis for Readmission Rates
| Predictor Variable | B | SE | β | t | p |
| Use of EHRs | -0.28 | 0.09 | -0.25 | -3.11 | 0.002 |
| Telehealth Services | -0.22 | 0.11 | -0.19 | -2.00 | 0.048 |
| Patient-Centered Care | -0.34 | 0.08 | -0.33 | -4.25 | <0.001 |
| Age | -0.06 | 0.05 | -0.08 | -1.20 | 0.232 |
| Gender | 0.03 | 0.07 | 0.03 | 0.43 | 0.667 |
| Years of Experience | -0.09 | 0.06 | -0.10 | -1.50 | 0.137 |
Table 5: Regression Analysis for Length of Hospital Stay
| Predictor Variable | B | SE | β | t | p |
| Use of EHRs | -0.32 | 0.08 | -0.30 | -4.00 | <0.001 |
| Telehealth Services | -0.29 | 0.09 | -0.26 | -3.22 | 0.002 |
| Patient-Centered Care | -0.38 | 0.07 | -0.39 | -5.43 | <0.001 |
| Age | -0.04 | 0.04 | -0.06 | -1.00 | 0.318 |
| Gender | 0.01 | 0.05 | 0.01 | 0.20 | 0.841 |
| Years of Experience | -0.11 | 0.05 | -0.13 | -2.20 | 0.029 |
The regression analyses indicate that the use of EHRs, telehealth services, and patient-centered care are significant predictors of improved patient satisfaction, reduced readmission rates, and shorter lengths of hospital stay. These findings highlight the positive impact of innovative nursing practices on patient outcomes.
4.4 Hypothesis Testing
The following hypotheses were tested based on the survey data:
- H1: The use of electronic health records (EHRs) is positively associated with improved patient satisfaction.
- H2: The implementation of telehealth services is negatively associated with readmission rates.
- H3: Patient-centered care models are negatively associated with the length of hospital stay.
The results of the correlation and regression analyses support all three hypotheses, indicating that these innovative practices significantly enhance patient outcomes.
4.5 Presentation of Mathematical Tables and Graphs
Table 1: Demographic Breakdown of Survey Participants
(See above for details)
Table 2: Correlation Analysis of Nursing Practices and Patient Outcomes
(See above for details)
Table 3: Regression Analysis for Patient Satisfaction
(See above for details)
Table 4: Regression Analysis for Readmission Rates
(See above for details)
Table 5: Regression Analysis for Length of Hospital Stay
(See above for details)
The quantitative analysis provides robust evidence supporting the positive impact of innovative nursing practices on patient outcomes. The use of electronic health records, telehealth services, and patient-centered care models are significantly associated with higher patient satisfaction, reduced readmission rates, and shorter lengths of hospital stay. These findings underscore the importance of adopting innovative practices in nursing management to enhance patient care. The next chapter will delve into the qualitative analysis, providing deeper insights through case studies and interviews. This comprehensive approach aims to further illuminate the practical implications of these innovations in diverse healthcare settings.
Chapter 5: Qualitative Analysis
5.1 Case Study 1: Implementation of Technology in Nursing Management
Background of the Healthcare Facility
The first case study focuses on a large urban hospital in London, known for its advanced implementation of healthcare technologies. This facility has been at the forefront of adopting electronic health records (EHRs) and other digital tools to enhance nursing management and patient care.
Description of the Technology and Its Implementation
The hospital implemented an integrated EHR system designed to streamline patient information management, enhance communication among healthcare providers, and improve the accuracy of medical records. The transition involved extensive training for nursing staff and a phased rollout to ensure minimal disruption to daily operations.
Impact on Nursing Practices and Patient Outcomes Interviews with nurse managers and staff nurses revealed that the EHR system significantly improved workflow efficiency and reduced medication errors. Nurses reported spending less time on administrative tasks and more time on direct patient care. Patient outcomes improved notably, with reductions in readmission rates and enhanced patient satisfaction scores.
5.2 Case Study 2: Patient-Centered Care Models
Background of the Healthcare Facility The second case study examines a community hospital in New York, recognized for its patient-centered care approach. This facility has implemented various strategies to prioritize patient needs and preferences, fostering a more personalized care environment.
Description of the Patient-Centered Care Model The hospital’s patient-centered care model includes multidisciplinary team meetings, personalized care plans, and active patient involvement in decision-making processes. The model also emphasizes the physical and emotional well-being of patients, integrating holistic care practices.
Staff and Patient Feedback on the New Care Model Interviews with staff and patients indicated high levels of satisfaction with the patient-centered approach. Nurses reported improved job satisfaction and engagement, as they felt more connected to their patients’ well-being. Patients expressed appreciation for the personalized care and reported feeling more valued and understood, contributing to improved overall health outcomes.
5.3 Case Study 3: Leadership and Management Innovations
Background of the Healthcare Facility The third case study investigates a leading healthcare institution in Lagos, Nigeria, renowned for its innovative leadership and management practices. This facility has embraced transformational leadership principles to drive improvements in nursing care.
Description of Leadership Strategies and Management Innovations The leadership strategies at this hospital focus on empowering nursing staff through continuous professional development, participative decision-making, and recognition of achievements. The management team has introduced initiatives such as mentorship programs and leadership workshops to cultivate a culture of excellence and innovation.
Evaluation of the Impact on Staff Performance and Patient Outcomes Interviews with nurse managers and staff nurses highlighted significant improvements in staff morale, teamwork, and professional growth. These leadership initiatives have fostered a positive work environment, resulting in enhanced patient care quality. Patients reported higher levels of satisfaction, and the hospital observed lower turnover rates among nursing staff.
5.4 Thematic Analysis of Interviews
Identification of Key Themes Thematic analysis of the interview data from the three case studies revealed several recurring themes:
- Enhanced Communication and Collaboration: Innovations in technology and leadership practices have significantly improved communication and collaboration among healthcare providers.
- Increased Efficiency and Reduced Errors: The adoption of EHRs and other digital tools has streamlined workflows, reduced administrative burdens, and minimized medication errors.
- Improved Patient Engagement and Satisfaction: Patient-centered care models have led to higher levels of patient engagement and satisfaction, as patients feel more involved in their care.
- Empowerment and Professional Development: Transformational leadership practices have empowered nursing staff, fostering professional growth and a culture of continuous improvement.
Discussion of Findings The findings from the qualitative analysis support the quantitative results, indicating that innovative practices in nursing management and care positively impact patient outcomes. Enhanced communication and collaboration were consistently mentioned as critical factors contributing to improved care quality. The integration of technology, particularly EHRs, was highlighted as a significant driver of efficiency and accuracy in nursing practices.
The patient-centered care model emerged as a powerful approach to improving patient satisfaction and health outcomes. By involving patients in their care decisions and addressing their holistic needs, healthcare facilities can foster a more supportive and healing environment. Leadership and management innovations, particularly those focusing on empowerment and professional development, were found to enhance staff performance and job satisfaction, ultimately leading to better patient care.
Conclusion
The qualitative analysis provides rich, contextual insights into the practical implementation and impact of innovative nursing practices. The case studies illustrate how technology, patient-centered care models, and transformational leadership can drive significant improvements in both nursing practices and patient outcomes. These findings align with the quantitative results, reinforcing the importance of adopting innovative approaches in nursing management.
The next chapter will discuss the integrated findings from both the quantitative and qualitative analyses, highlighting their implications for nursing practice and policy. This comprehensive approach aims to provide actionable insights that can enhance nursing practices and optimize patient outcomes in diverse healthcare settings.
N.B.: For confidentiality purposes, the names of the healthcare facilities and individuals involved in this study have been withheld as requested by the participants.
Chapter 6: Discussion
6.1 Interpretation of Quantitative Findings
The quantitative analysis of this study demonstrated a significant positive impact of innovative nursing practices on patient outcomes. The use of electronic health records (EHRs), telehealth services, and patient-centered care models were strongly correlated with improved patient satisfaction, reduced readmission rates, and shorter lengths of hospital stay. These findings are consistent with existing literature, highlighting the critical role of technology and patient-centered approaches in enhancing healthcare delivery. For instance, Bates et al. (2018) found that the implementation of EHRs led to improved accuracy of patient data and better coordination of care, which aligns with our study’s findings on the positive effects of EHRs on patient outcomes.
6.2 Interpretation of Qualitative Findings
The qualitative analysis provided in-depth insights into the practical implementation and impacts of innovative nursing practices. The case studies and interviews revealed that the adoption of EHRs, patient-centered care models, and transformational leadership practices significantly enhanced communication, collaboration, and efficiency among healthcare providers. Staff and patient feedback highlighted the benefits of these innovations in creating a more supportive and effective care environment. For example, the patient-centered care model at the community hospital in New York resulted in higher levels of patient engagement and satisfaction, mirroring the quantitative findings on patient-centered approaches.
6.3 Synthesis of Quantitative and Qualitative Results
Combining the quantitative and qualitative findings, it is evident that innovative nursing practices not only improve patient outcomes but also enhance the overall healthcare environment. The quantitative data provided robust statistical evidence of the benefits of these practices, while the qualitative insights offered a deeper understanding of how these innovations are implemented and experienced by healthcare professionals and patients. The integration of these methods allowed for a comprehensive analysis, confirming that innovations like EHRs, telehealth, and patient-centered care models contribute to better healthcare delivery and patient outcomes.
6.4 Implications for Nursing Management
The findings of this study have several important implications for nursing management. First, the positive impact of EHRs and other digital tools underscores the need for healthcare facilities to invest in technology infrastructure and provide adequate training for nursing staff. Ensuring that nurses are proficient in using these tools can lead to significant improvements in efficiency and patient care quality. Additionally, the benefits of patient-centered care models suggest that nursing managers should prioritize strategies that actively involve patients in their care, fostering a more personalized and responsive healthcare experience.
6.5 Implications for Patient Care
From a patient care perspective, the adoption of innovative practices can lead to substantial improvements in patient outcomes and satisfaction. The emphasis on personalized care and effective communication helps build trust and rapport between patients and healthcare providers, which is crucial for successful treatment and recovery. Telehealth services can extend the reach of healthcare services to underserved populations, improving access to care and continuity of treatment. Nursing practices that incorporate these innovations are better positioned to meet the diverse needs of patients and deliver high-quality care.
6.6 Theoretical Contributions
This study contributes to the theoretical understanding of nursing management and patient care by integrating various theoretical models and empirical evidence. The Health Belief Model (Champion & Skinner, 2008) and the Donabedian Model of Quality Care (Ayanian & Markel, 2016) provided a strong foundation for examining how innovative practices influence patient behaviors and outcomes. Lewin’s Change Management Theory (Cummings, Bridgman, & Brown, 2016) helped explain the dynamics of implementing these changes in healthcare settings. By applying these frameworks, this research enhances the theoretical understanding of how innovations in nursing can lead to better patient outcomes and more effective healthcare management.
6.7 Practical Recommendations
Based on the findings, several practical recommendations can be made for nursing managers and healthcare providers:
- Invest in Technology: Healthcare facilities should prioritize investments in technology, such as EHRs and telehealth services, to enhance efficiency and patient care quality. Training programs should be implemented to ensure that nursing staff are proficient in using these tools.
- Adopt Patient-Centered Care Models: Nursing managers should implement patient-centered care models that actively involve patients in their care decisions. This approach can lead to higher patient satisfaction and better health outcomes.
- Promote Transformational Leadership: Leadership training programs that focus on transformational leadership principles can empower nursing staff, improve job satisfaction, and enhance overall care quality.
- Foster Interprofessional Collaboration: Encouraging collaboration among different healthcare professionals can improve communication and coordination, leading to more comprehensive and effective patient care.
The discussion involves the quantitative and qualitative findings, providing a comprehensive understanding of the impact of innovative nursing practices on patient outcomes. The integration of technology, patient-centered care models, and transformational leadership significantly enhances nursing management and patient care, leading to improved patient satisfaction, reduced readmission rates, and shorter hospital stays. These findings underscore the importance of adopting innovative approaches in nursing practice to meet the evolving needs of patients and the healthcare system. The practical recommendations provided can guide healthcare facilities in implementing these innovations effectively, ultimately contributing to better patient outcomes and more efficient healthcare delivery.
Chapter 7: Conclusion
7.1 Summary of Key Findings
This research sought to find out the impact of innovative nursing practices on patient outcomes, employing a mixed-methods approach that combined quantitative surveys and qualitative case studies. The study identified key innovative practices, including the use of electronic health records (EHRs), telehealth services, and patient-centered care models, which have significantly improved patient outcomes. The quantitative analysis revealed strong positive correlations between these practices and enhanced patient satisfaction, reduced readmission rates, and shorter lengths of hospital stay. The qualitative insights provided deeper understanding of the practical implementation and benefits of these innovations, highlighting improvements in workflow efficiency, communication, and patient engagement.
7.2 Limitations of the Study
While this study provides valuable insights, it is not without limitations. The sample size, although sufficient for statistical analysis, may not be representative of all healthcare settings. The study primarily focused on large urban hospitals and may not fully capture the experiences of smaller or rural healthcare facilities. Additionally, the cross-sectional design of the survey limits the ability to draw causal inferences. Longitudinal studies would be necessary to confirm the long-term effects of these innovative practices on patient outcomes.
7.3 Recommendations for Practice
Based on the findings, several recommendations can be made for nursing managers and healthcare providers. First, there should be a concerted effort to invest in and adopt technological advancements such as EHRs and telehealth services. These tools not only enhance efficiency but also improve patient care quality. Second, implementing patient-centered care models should be prioritized, as these models significantly enhance patient satisfaction and engagement. Third, fostering a culture of transformational leadership within nursing teams can lead to higher staff morale and better patient outcomes. Leadership training and continuous professional development should be integral components of nursing management strategies.
7.4 Directions for Future Research
Future research should aim to address the limitations identified in this study. Larger, more diverse samples that include various types of healthcare settings would provide a more comprehensive understanding of the impact of innovative practices. Longitudinal studies are needed to examine the long-term effects of these practices on patient outcomes and healthcare costs. Additionally, future research could explore the role of cultural and contextual factors in the successful implementation of innovative nursing practices. Understanding these factors could help tailor strategies to different healthcare environments, enhancing the effectiveness of these innovations.
7.5 Final Thoughts
In conclusion, this study has demonstrated the significant positive impact of innovative nursing practices on patient outcomes. The integration of technology, patient-centered care, and transformational leadership practices are essential components of modern nursing management that drive improvements in healthcare delivery. While challenges remain, the benefits of adopting these innovations are clear. By investing in these practices and fostering an environment that supports continuous improvement and innovation, healthcare providers can enhance patient care, improve outcomes, and contribute to a more efficient and effective healthcare system.
As the healthcare landscape continues to evolve, it is imperative for nursing managers and healthcare leaders to stay abreast of emerging trends and technologies. Embracing innovation and adapting to change will be crucial for meeting the growing demands of patient care and ensuring that healthcare systems remain resilient and responsive. The insights gained from this study provide a solid foundation for ongoing efforts to optimize nursing practices and patient outcomes, ultimately leading to a healthier and more satisfied patient population.
References
Ayanian, J. Z., & Markel, H. (2016). Donabedian’s Lasting Framework for Health Care Quality. New England Journal of Medicine, 375(3), 205-207.
Baig, M. M., GholamHosseini, H., & Connolly, M. J. (2019). Mobile healthcare applications: System design review, critical issues and challenges. Australasian Physical & Engineering Sciences in Medicine, 42(4), 615-625.
Bates, D. W., Sheikh, A., Asch, D. A. (2018). Innovative Uses of Electronic Health Records and Health Information Technology to Improve Patient Care. Annual Review of Medicine, 69(1), 51-65.
Boamah, S. A., Spence Laschinger, H. K., Wong, C., & Clarke, S. (2018). Effect of transformational leadership on job satisfaction and patient safety outcomes. Nursing Outlook, 66(2), 180-189.
Champion, V. L., & Skinner, C. S. (2008). The Health Belief Model. In Health Behavior and Health Education: Theory, Research, and Practice (4th ed., pp. 45-65). Jossey-Bass.
Chien, L. Y. (2019). Evidence-based practice and nursing research. Journal of Nursing Research, 27(5), e29.
Collins, F. S., & Varmus, H. (2015). A New Initiative on Precision Medicine. New England Journal of Medicine, 372(9), 793-795.
Cummings, S., Bridgman, T., & Brown, K. G. (2016). Unfreezing change as three steps: Rethinking Kurt Lewin’s legacy for change management. Human Relations, 69(1), 33-60.
Kruse, C. S., Karem, P., Shifflett, K., Vegi, L., Ravi, K., & Brooks, M. (2018). Evaluating barriers to adopting telemedicine worldwide: A systematic review. Journal of Telemedicine and Telecare, 24(1), 4-12.
Olsson, L. E., Jakobsson Ung, E., Swedberg, K., & Ekman, I. (2016). Efficacy of person-centred care as an intervention in controlled trials – a systematic review. Journal of Clinical Nursing, 25(3-4), 456-466.
Reeves, S., Fletcher, S., Barr, H., Birch, I., Boet, S., Davies, N., … & Kitto, S. (2017). A BEME systematic review of the effects of interprofessional education: BEME Guide No. 39. Medical Teacher, 38(7), 656-668.
Santana, M. J., Manalili, K., Jolley, R. J., Zelinsky, S., Quan, H., & Lu, M. (2018). How to practice person-centred care: A conceptual framework. Health Expectations, 21(2), 429-440.